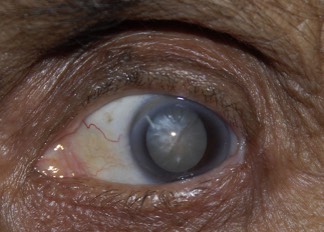
Modern cataract surgery is one of the safest and most effective of all operations. 99 times out of 100 you will see better, and usually by the next day. No surgery is totally without risk however, and it is important for any patient to understand what can go wrong such that they can make an informed decision to have the surgery. I have summarised the risks and their comparative frequency below. Some of the complications are treatable and should not affect your end result. Other complications are more serious and can damage your vision. Taking all the risks into account the overall chance of your vision being made significantly worse by cataract surgery is about 1 in 1000.
If any bacteria enter the eye at the time of surgery this can lead to an intra-ocular infection. While often treatable, the infection can still sometimes damage the vision. The rate of infection is minimised with strict sterile technique at the time of surgery.
The tiny blood vessels in the retina can bleed at the time of surgery. This can lead to scarring of the retina and a reduction in your vision. If you are diabetic, it is very important to make sure your retina is fully treated prior to any cataract surgery.
If the cataract lens slides through a ruptured posterior capsule into the vitreous (the jelly that fills the main cavity of the eye) then you will need secondary surgery by a vitreo-retinal specialist to remove the cataract. The end result can still be perfect but with the same problems of lens fixation as for any ruptured capsule and with the additional risks of the extra surgery.
There is an increased risk of retinal detachment for the months following cataract surgery. This risk is greater for patients with myopia (short sight).
If the lens capsule is ruptured at the time of surgery it will be difficult to fit your intra-ocular lens. In some circumstances the lens can be placed on the rim of the capsule, in some circumstances the lens can be clipped to your iris and in some circumstances the lens may need to be placed in front of the iris. While the result can still be perfect the surgery will have been more complex, your recovery may be delayed and there is a greater risk of the lens de-centring with a worse visual outcome.
The artificial lens placed into your eye is chosen based on pre-operative measurements. Sometimes the lens does not give the expected result and as a result your eye ends up either slightly long or short sighted. If the outcome is significant there are a number of options. The lens can be removed and replaced. A secondary intra-ocular lens can be placed over the lens to correct the refractive error. The cornea can be treated with laser surgery or you could wear either contact lenses or glasses.
The retina can swell up due to the surgery. This can reduce your vision. You may need to take additional drops for a longer period. The condition usually improves over some weeks to months, if it does not resolve your central vision can remain blurred.
The outer layer of your old lens is kept to act as a carrier bag for your new lens. This layer can itself thicken. This typically occurs one to two years later and gives the same symptoms as the original cataract. The treatment is straightforward and involves cutting a hole in this layer with a YAG laser. As the treatment is very simple and effective we do not really consider this a risk of cataract surgery, rather more of a nuisance which we are continuing to minimise with modern lens design.